MDMA psychiatric applications synthesized: comprehensive review examines PTSD treatment and emerging therapeutic targets
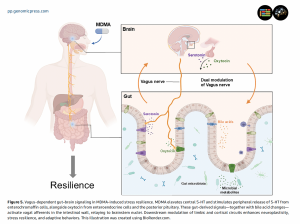
Vagus-dependent gut–brain signaling inMDMA-induced stress resilience. MDMA elevates central 5-HT and stimulates peripheral release of 5-HT from enterochromaffin cells, alongside oxytocin from enteroendocrine cells and the posterior pituitary. These gut-de
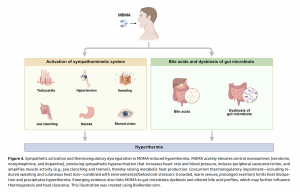
Sympathetic activation and thermoregulatory dysregulation in MDMA-induced hyperthermia. MDMA acutely elevates central monoamines (serotonin, norepinephrine, and dopamine), producing sympathetic hyperactivation that increases heart rate and blood pressure,
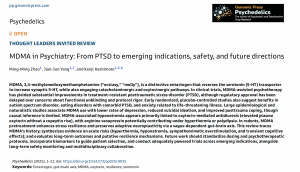
A comprehensive peer-reviewed invited review published today in Psychedelics synthesizes the evolving landscape of MDMA-assisted psychotherapy.
Historical Context and Chemical Origins. The synthesis begins with MDMA's origins at Merck in 1912, where chemist Anton Köllisch first created the compound as an intermediate in developing hemostatic agents. Originally designated as "Methylsafrylamin" and "Safrylmethylamin," the substance remained essentially dormant until Alexander Shulgin rediscovered its unique psychoactive properties in the 1970s. The review documents how between the late 1970s and early 1980s, pioneering psychotherapists including George Greer and Requa Tolbert began incorporating MDMA into therapeutic sessions, reporting pronounced improvements in mood, social functioning, and psychological insight following single sessions.
The authors detail the critical transition period of the mid-1980s when escalating recreational use prompted the Drug Enforcement Administration to classify MDMA as Schedule I in 1985, effectively halting clinical research for nearly two decades. This regulatory action occurred despite protests from psychiatrists who argued for its therapeutic value, creating what the authors describe as a significant gap in psychiatric treatment development.
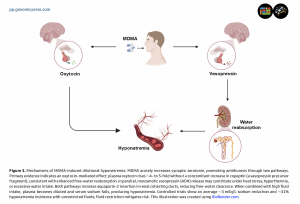
Bridging Seven Decades of Research. The review encompasses MDMA research spanning from its 1912 synthesis at Merck through contemporary Phase III clinical trials, representing one of the most thorough temporal analyses of this compound to date. Dr. Hashimoto and colleagues systematically analyze how this distinctive entactogen reverses the serotonin transporter to massively increase synaptic serotonin while simultaneously engaging oxytocin and catecholaminergic pathways. Through examination of 126 primary sources, the authors construct a comprehensive narrative demonstrating how MDMA produces its unique prosocial and therapeutic effects through multiple interconnected neurobiological systems.
The pharmacological analysis reveals MDMA's primary mechanism involves reversing the serotonin transporter (SERT), causing massive serotonin efflux that underlies acute mood elevation, anxiolysis, and empathogenic effects. Recent studies highlighted in the review demonstrate that genetic or pharmacological blockade of SERT or specific serotonin receptors in the nucleus accumbens abolishes MDMA-induced social affiliation, while dopaminergic signaling mediates rewarding effects. Particularly noteworthy findings show that MDMA's robust serotonin release actively restrains its own dopamine-mediated reinforcement potential, explaining its lower abuse liability compared to methamphetamine despite similar dopamine-releasing capacity.
This synthesis arrives at a critical juncture following the FDA's August 2024 decision requesting additional Phase III trials despite earlier Breakthrough Therapy designation granted in 2017. The review methodically addresses concerns about functional unblinding and protocol standardization that contributed to regulatory delays while maintaining focus on the substantial therapeutic potential demonstrated across multiple psychiatric conditions. The authors note that approximately 90 percent of participants receiving active drug and 75 percent receiving placebo correctly identified their treatment assignment, raising fundamental questions about conducting truly blinded trials with psychoactive substances.
Convergent Evidence Across Psychiatric Indications. The authors identify consistent therapeutic patterns across diverse clinical applications, with PTSD trials showing particularly robust outcomes that have captured international attention. Phase II and III studies demonstrated remission rates approaching 80 percent in treatment-resistant cases, with therapeutic benefits persisting for years following treatment completion. The synthesis reveals how MDMA-assisted therapy achieved significant symptom reductions in populations where conventional approaches including selective serotonin reuptake inhibitors, cognitive behavioral therapy, and prolonged exposure therapy had failed.
The review provides detailed analysis of the pivotal trials conducted by the Multidisciplinary Association for Psychedelic Studies (now Lykos Therapeutics). The first randomized controlled trial in 2010 treated 20 patients with chronic treatment-resistant PTSD, achieving an 80 percent remission rate maintained at three-year follow-up. Subsequent trials in military veterans, first responders, and civilian populations consistently demonstrated effect sizes substantially exceeding those of conventional PTSD treatments.
Beyond PTSD, the review synthesizes emerging evidence across multiple psychiatric conditions. In autism spectrum disorder, controlled trials demonstrated significant reductions in social anxiety, with participants reporting improved capacity for social connection and reduced fear of interpersonal interaction. The authors analyze how MDMA's oxytocin-mediated effects may specifically address core social deficits characteristic of autism, offering a mechanism-based approach where traditional interventions have shown limited efficacy.
Similarly promising signals emerge from studies examining eating disorders with comorbid PTSD. The review details how MDMA-assisted therapy significantly reduced eating disorder symptomatology in addition to trauma symptoms, suggesting potential for addressing the complex interplay between trauma and disordered eating behaviors. In patients experiencing existential distress from life-threatening illness, preliminary trials show substantial reductions in anxiety and depression sustained for months after treatment.
Novel Gut-Brain Mechanisms of Resilience. A particularly innovative contribution involves the authors' synthesis of recent discoveries regarding MDMA-induced resilience through vagus nerve-dependent gut-brain signaling, representing a paradigm shift in understanding MDMA's therapeutic mechanisms. The review integrates findings from multiple preclinical studies demonstrating that MDMA pretreatment prevents stress-induced behavioral and neurobiological changes through modulation of gut microbiota composition and bile acid metabolism.
The authors detail how approximately 90 percent of the body's serotonin is synthesized by enterochromaffin cells in the gastrointestinal tract, where it regulates intestinal function while signaling to both enteric and central nervous systems. Preclinical studies reveal that MDMA administration preserves adaptive neuroplasticity and prevents depression-like behaviors in chronic stress models through mechanisms requiring intact vagal signaling.
Subdiaphragmatic vagotomy abolishes both MDMA-induced oxytocin release and its resilience-enhancing effects, establishing the vagus nerve as critical for therapeutic action.
Recent research highlighted in the review demonstrates that repeated intermittent MDMA administration significantly reduced demyelination in cuprizone-treated mice, with gut microbiota analysis revealing specific bacterial changes correlating with neuroprotection. The synthesis connects these findings to epidemiological data associating MDMA use with reduced depression and suicidality at population levels, though the authors carefully note limitations in establishing causality from observational studies.
Critical Safety Considerations and Risk Mitigation. The review provides the most comprehensive analysis to date of acute and chronic safety concerns associated with MDMA administration. The authors synthesize evidence demonstrating that controlled trials show an average 3 milliequivalent per liter sodium reduction with unrestricted fluid intake, with approximately 31 percent of participants developing hyponatremia. They identify oxytocin-mediated antidiuresis as the primary mechanism while noting arginine vasopressin contributions under specific conditions including hyperthermia or excessive water consumption.
The detailed safety analysis reveals that hyperthermia represents the most serious acute risk, with the authors describing novel findings linking MDMA-induced temperature dysregulation to gut microbiota-derived bile acids. A groundbreaking study detailed in the review showed that microbiome depletion converted MDMA's hyperthermic effect into a hypothermic response, suggesting gut bacteria play essential roles in thermoregulation during MDMA exposure.
Regarding neurotoxicity concerns, the synthesis examines convergent evidence from human neuroimaging studies, cognitive assessments, and animal models demonstrating selective serotonergic terminal injury amplified by hyperthermia and oxidative stress. Positron emission tomography studies in abstinent MDMA users consistently show reduced serotonin transporter availability throughout cortical and subcortical regions, alongside compensatory upregulation of postsynaptic receptors. The authors emphasize how controlled clinical settings with temperature monitoring, fluid restriction, and dosing limits can substantially mitigate these risks while preserving therapeutic benefits.
Framework for Clinical Translation and Regulatory Considerations. The review proposes specific strategies for advancing MDMA-assisted therapy toward clinical implementation despite recent regulatory setbacks. The authors advocate for incorporating biomarkers including threat-evoked functional magnetic resonance imaging and oxytocin receptor genotyping to guide patient selection and predict treatment response. They emphasize the critical need for standardizing both pharmacological protocols and psychotherapeutic components while developing consensus on acceptable unblinding thresholds in controlled trials.
The analysis addresses the FDA's concerns about functional unblinding directly, noting that the pronounced subjective effects of MDMA make traditional placebo controls problematic. The authors discuss potential solutions including active placebo comparators, dose-response designs, and independent rater assessments to minimize bias while acknowledging that some degree of unblinding may be inevitable with psychoactive interventions.
International Developments and Future Directions. The review documents significant international developments, including Australia's Therapeutic Goods Administration reclassification of MDMA to Schedule 8 in July 2023, permitting qualified psychiatrists to prescribe MDMA-assisted therapy under strict protocols. This regulatory approval, the first of its kind globally, has prompted intense debate about appropriate evidence thresholds for approving psychedelic-assisted therapies.
Dr. Hashimoto, Professor at Chiba University Center for Forensic Mental Health, brings extensive expertise in neuropharmacology and stress resilience mechanisms spanning three decades of research. The international team combines clinical psychiatry experience from leading medical centers in China with fundamental neuroscience perspectives, positioning them uniquely to synthesize this complex, multidisciplinary field. Dr. Jian-Jun Yang from The First Affiliated Hospital of Zhengzhou University contributes expertise in anesthesiology and perioperative medicine, while the team's collective work has advanced understanding of neuroplasticity and psychiatric treatment mechanisms.
Implications for Clinical Practice and Research. The comprehensive review article represents a critical synthesis of the current state of knowledge in MDMA-assisted psychotherapy, providing researchers, clinicians, and policymakers with an evidence-based framework for understanding this emerging therapeutic modality. By systematically analyzing and integrating findings from across the literature, the authors offer both a historical perspective on how the field has evolved and a detailed roadmap for future investigations.
The synthesis emphasizes that achieving MDMA's full therapeutic promise will require unprecedented collaboration among neuroscientists, clinicians, psychotherapists, ethicists, and regulators. The authors call for well-powered, rigorously designed studies across autism spectrum disorder, eating disorders, and other conditions, paired with mechanistic research on microbiota-mediated effects, vagal signaling, and receptor-specific actions. They stress that longitudinal monitoring of cognition, neuroimaging changes, and adverse event patterns will be essential for defining long-term risk-benefit profiles and developing evidence-based clinical guidelines.
Such comprehensive reviews are essential for identifying patterns that may not be apparent in individual studies, resolving apparent contradictions in the literature, and highlighting the most promising avenues for advancing the field. The synthesis presented here serves as a valuable resource for both newcomers seeking to understand the field and experienced researchers looking to contextualize their work within the broader scientific landscape, while providing regulatory bodies with consolidated evidence to inform policy decisions.
The peer-reviewed Thought Leaders Invited Review in Psychedelics titled "MDMA in Psychiatry: From PTSD to emerging indications, safety, and future directions," is freely available via Open Access on 14 October 2025 in Psychedelics at the following hyperlink: https://doi.org/10.61373/pp025i.0035.
About Psychedelics: Psychedelics: The Journal of Psychedelic and Psychoactive Drug Research (ISSN: 2997-2671, online and 2997-268X, print) is a peer reviewed medical research journal published by Genomic Press, New York. Psychedelics is dedicated to advancing knowledge across the full spectrum of consciousness altering substances, from classical psychedelics to stimulants, cannabinoids, entactogens, dissociatives, plant derived compounds, and novel compounds including drug discovery approaches. Our multidisciplinary approach encompasses molecular mechanisms, therapeutic applications, neuroscientific discoveries, and sociocultural analyses. We welcome diverse methodologies and perspectives from fundamental pharmacology and clinical studies to psychological investigations and societal-historical contexts that enhance our understanding of how these substances interact with human biology, psychology, and society.
Visit the Genomic Press Virtual Library: https://issues.genomicpress.com/bookcase/gtvov/
Our full website is at: https://genomicpress.kglmeridian.com/
Ma-Li Wong
Genomic Press
mali.wong@genomicpress.com
Visit us on social media:
LinkedIn
Bluesky
Instagram
Facebook
X
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.